Acne is one of the most common skin concerns seen in the treatment room, affecting up to 50 million Americans annually. Yet while it often presents as a simple breakout on the surface, not all acne behaves—or responds—the same way.
Different biological processes influence how acne forms, from sebum activity to congestion to inflammation. Understanding these distinctions gives you clearer insight into what’s happening beneath the surface and helps you guide patients toward consistent, supportive care.
When patients understand why their skin behaves the way it does, they’re more likely to stay committed to both professional treatments and home routines. Below, we break down the most common categories and how each shows up in the skin.
Non-Inflammatory Acne (Comedonal Acne)
Non-inflammatory acne typically represents the earliest stage of congestion. These lesions are rooted in buildup within the follicle—not redness, swelling, or visible irritation.
Blackheads (Open Comedones)
Appear as small dark dots, most commonly on the nose, chin, and forehead
Dark color results from oxidation when debris in an open pore is exposed to oxygen
Can create the appearance of uneven or shadowed texture
Whiteheads (Closed Comedones)
Small, firm bumps just beneath the surface
Because the pore is closed, they often look white or flesh-colored
Common in the T-zone and contribute to a rough or uneven look
In the treatment room:
Focus on gentle exfoliation, hydration, and barrier support. Consistent professional maintenance helps refine the look of surface texture without overstimulating the skin.
Inflammatory Acne
Inflammatory acne occurs when congestion is accompanied by redness, swelling, or discomfort. At the cellular level, this happens when naturally present bacteria multiply within a blocked pore and trigger an inflammatory cascade.
Papules
Small, red, tender bumps
No visible center
Often the earliest sign of inflammation around the follicle
Pustules
Similar to papules, but develop a white or yellow center
Slightly raised with fluid closer to the surface
Often appear in clusters
Nodules
Larger, firm lesions deeper within the skin
Can persist for weeks
May leave temporary post-inflammatory marks once resolved
Cysts
Deep, fluid-filled lesions that feel swollen or tender
May not always be highly visible on the surface
Can affect comfort and contribute to uneven texture
In the treatment room:
Avoid friction and aggressive exfoliation. Prioritize calming, hydration, and restoring balance. With inflammatory presentations, consistency matters more than intensity.
What Actually Causes Acne?
Acne is multifactorial—meaning several influences interact at once. Common contributing factors include:
Excess sebum that clogs the follicle opening
Slower cellular turnover leading to buildup
Environmental stressors like humidity or pollution
Product habits or lifestyle factors that occlude the skin or disrupt balance
Helping patients understand this foundation reframes the conversation from “quick fixes” to long-term consistency and intentional care.
When teaching patients about acne, a clear, observational approach builds trust. Identifying whether the primary concern is comedonal or inflammatory helps you tailor both service planning and at-home recommendations.
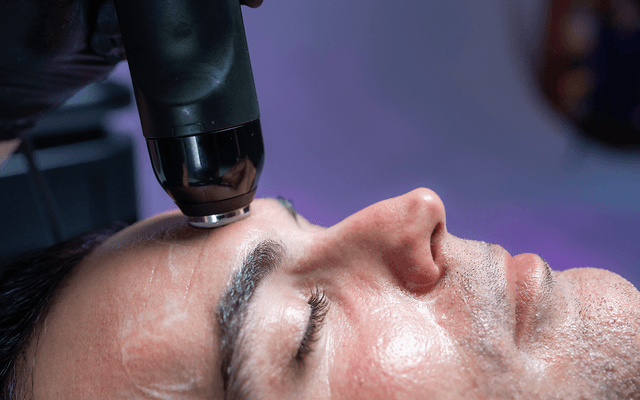
Visual aids—charts, imagery, controlled before-and-after photos—can help patients correctly interpret what they see in the mirror. Many interpret general congestion or sensitivity as “breakouts,” when the underlying issue may be buildup, dehydration, or barrier imbalance.
Progress with acne is steady, not immediate. While professional treatments can visibly improve clarity, texture, and comfort, long-term change requires routine and patience.
Encourage patients to look for:
Smoother texture
Less visible redness
A more even appearance
Fewer flare-ups over time
Patients who feel informed and supported are far more likely to remain consistent and achieve visible balance.
FAQs
Is acne always caused by bacteria?
Not always. While bacteria can contribute to inflammation, many forms of acne—especially comedonal—stem from buildup, oil activity, or slower cellular turnover.
Can dehydration make breakouts appear worse?
Yes. A compromised barrier can exaggerate the look of congestion and make inflammation appear more pronounced.
How long does it take for patients to see progress?
Most patients notice smoother texture and less visible redness within several weeks of consistent care. Deeper lesions may take longer to visibly improve.
Should patients exfoliate more often if they have breakouts?
Not necessarily. Over-exfoliation can compromise the barrier and worsen visible inflammation. Gentle, consistent routines are more supportive than aggressive ones.